Long-term COVID-19 Data Surveillance Is an International Responsibility
Many countries have benefitted from access to others’ COVID-19 data to identify risks ahead of time and adequately prepare their systems. This cross-border collaboration cannot end once COVID-19 becomes endemic. We must remain vigilant and continue collecting and analyzing data together.
While last week we discussed the importance of ongoing domestic COVID-19 surveillance, there was one signal that we omitted from the conversation – international data. Throughout this pandemic we have relied upon international trends and experiences to inform U.S. policy and public health responses before the various variant waves subsequently hit home. In fact, the entire Johns Hopkins Coronavirus Resource Center mission began with the COVID-19 Global Map, which remains one of the most trusted and reliable sources for aggregate international data across the globe. As we have said before, due to the interconnected nature of the world today, no one is safe from health threats until everyone is safe.
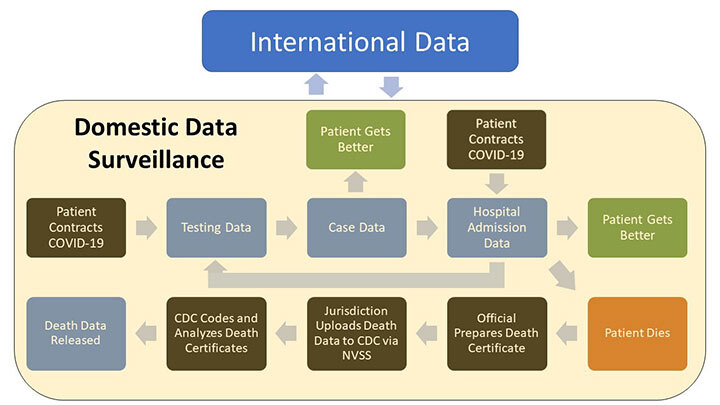
Instituting a domestic COVID-19 surveillance system is critical because, in addition to informing and protecting us, it can provide data to our partners around the world. Likewise, we will benefit from access to data from other countries. This equally beneficial partnership has the potential to provide data that could allow us to act far before our own testing, case, and hospitalization data would. In fact, this has often been the case throughout the COVID-19 pandemic.
With the SARS-CoV-2 virus first appearing in Asia, and major variants originating in Europe and Africa, the United States has relied heavily on international COVID-19 data. We could assess trends, study virus biology (transmissibility, severity), and design effective mitigation efforts before the variants spread stateside. As demonstrated in the image below comparing peaks for some of the major variants, the United States had a multi-week lead time to prepare for Delta based on data coming from many countries, including the United Kingdom and Japan as examples.
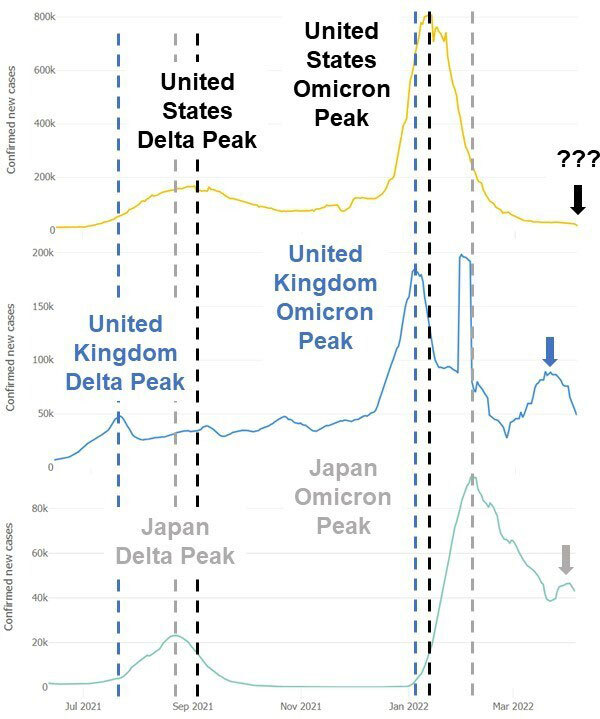
Similarly, with the Omicron variant, the disease burden peaked earlier in the United States and the United Kingdom, allowing Japan to prepare its resources for the overwhelming impact of Omicron. Now, experts are analyzing recent upticks in COVID-19 cases seen globally, which are also shown above in Japan and the United Kingdom. Trends have not yet shifted in the United States, but previous experiences show that it may be worth preparing for an increase in cases.
Clearly, international data has been an incredible tool throughout the COVID-19 pandemic, but do we have the ability to maintain this global collaboration after the crisis is over and COVID-19 becomes endemic? Yes, and we’ve done it before. Influenza is one of the most established examples. The World Health Organization (WHO) created the Global Influenza Surveillance and Response System (GISRS) in 1952 as a “global mechanism of surveillance, preparedness and response for seasonal, pandemic and zoonotic influenza.”1 The GISRS network covers 124 countries (below) and could be an incredible model for international collaboration on long-term COVID-19 surveillance.
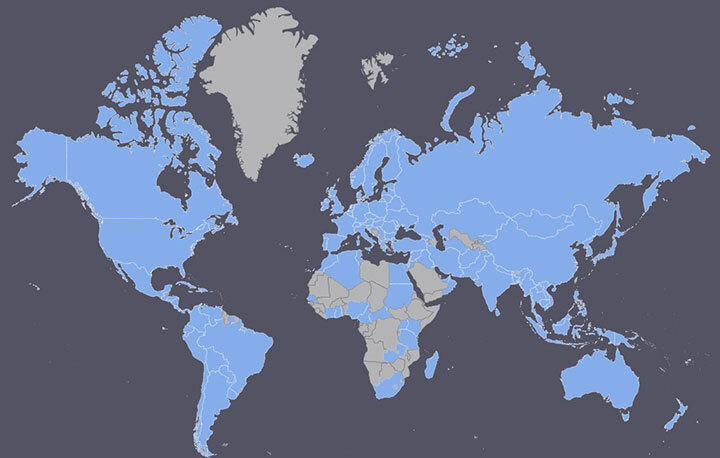
As demonstrated by the work of the GISRS, surveillance has many purposes apart from recording disease spread. Influenza samples from disease surveillance labs across the globe are analyzed to better understand virus biology, sequence variants, and identify any new viruses present. This data can influence the design and rollout of annual influenza vaccines as primary variants are identified. Additionally, epidemiological monitoring of testing and case data can serve as an early warning system for hospitals. Instead of reacting to a crisis while emergency rooms are overwhelmed, hospitals could prepare by shifting resources, obtaining personal protective equipment and instrumentation, and hiring or transferring staff when they are alerted that a new threat is on the way.
In addition to the WHO’s GISRS model of centralizing data from multi-national laboratories, each country can (and should) continue to release publicly available data on COVID-19, even possibly extending that release to include public data for other diseases like influenza. The CRC’s COVID-19 Global Map operates by scraping data from the public sources each country provides. We will continue to do so while most countries make these data available. However, if there is no global push for public infectious disease data, we will need a more formal plan and data sharing agreements.
Regardless of how we decide to collect and report data on COVID-19, there will be a need to establish and continually fund an international network of labs to analyze samples. COVID-19 data collection could possibly be combined with ongoing WHO efforts, or countries could commit to maintaining the labs they set up during the COVID-19 pandemic to analyze viral samples. There is also a role academia could play with access to sequencing and other molecular biology technologies, funding, and a proven spirit of collaboration. Wealthier countries will need to show their commitment to this cause and offer funds and support those without sufficient resources to field a permanent COVID-19 surveillance system. Eight of the top 25 countries for sequencing COVID-19 samples are considered developing nations, demonstrating that this capacity is not solely relegated to wealthier nations and that everyone can contribute to a global surveillance effort.
The United States can lead by example, continuing to make its COVID-19 data publicly available to serve as a warning system for other countries. We can also begin discussions and negotiations at the international level about long-term disease surveillance infrastructure. We can commit funds to the WHO to help countries with fewer resources establish labs and staff them. Congress has already declined to fund international vaccination efforts,2 and we cannot let the trend of isolationism continue in the realm of public health. With a unified effort, we can prevent future COVID-19 outbreaks, reinforce current infectious disease surveillance, and catch future pandemics before they even start. We may not all be in the same boat, but we’re in the same storm and can navigate it better together.
References
1. World Health Organization, Global Influenza Surveillance and Response System (GISRS). https://www.who.int/initiatives/global-influenza-surveillance-and-response-system. (Accessed 05 April 2022).
2. E. Cochrane, A.E. Petri, A.J. Khan, Covid News: Senators Announce Smaller Aid Proposal Without Global Vaccine Funds, The New York Times, 04 April 2022.
